Elizabeth Hofheinz, M.P.H., M.Ed.
New work from a Level 1 trauma center, Harbor-UCLA Medical Center in Torrance, California, has looked at 18 patients who underwent surgery for an isolated, displaced patella fracture between 2014 and 2018. The study, “Functional Outcomes of Patella Fractures Treated With Anterior Plate Osteosynthesis at One Year,” appears in the January 20201 edition of the Journal of Orthopaedic Trauma.
Co-author Stephen J. Shymon, M.D. is an orthopedic surgeon with Harbor-UCLA Medical Center. Dr. Shymon told OSN, “Clinically, we were noticing a high incidence of hardware irritation and hardware removal in patella fractures treated with tension band constructs involving Kirschner wires or cannulated screws.”
Finding a lack of literature on functional outcomes of anterior plate fixation for operative patella fractures at 1-year postop, the researchers dove in and assessed 18 patients, all of whom were treated by a senior orthopedic trauma surgeon.
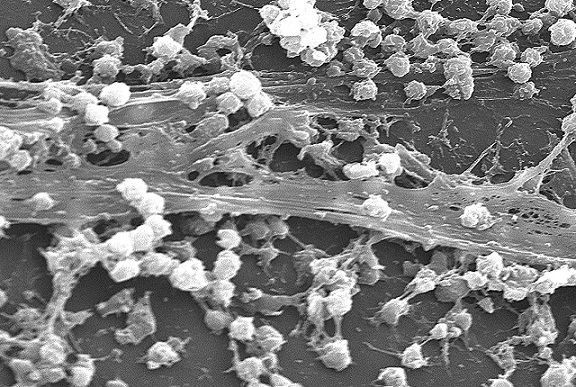
“Using a longitudinal midline incision over the patella, full- thickness flaps were elevated to minimize wound complications,” wrote the authors. “Fracture reduction was obtained using a variety of clamps, manual manipulation, and temporary fixation with K-wires. When the clamp obstructed the optimal plate position, either 2 additional clamps placed orthogonal to the fracture out of the way of the plate were placed to allow for removal of the obstructing clamp or K-wires were placed out of the way of the plate to provisionally stabilize the fracture reduction while the clamp was removed. Anterior plating was performed with either one or two 2.4/2.7-mm locking plates. Twelve patients had Synthes mini fragment plates, and 6 had Smith and Nephew EVOS plates. Plates were contoured to the patella and held provisionally while one or two 2.4/2.7-mm interfragmentary lag screws are placed through the most superior or inferior hole in the plate longitudinally across the patella.”
“When contouring the plate around the superior or inferior pole of the patella, a vertical incision is made in line with the quadriceps or patellar tendon insertion to allow the plate to lie directly on the bone. The vertical incision in the tendon is closed over the plate with absorbable suture at closure. Several unicortical 2.4/2.7-mm locking screws are then inserted into the plate to complete the construct. Depending on the senior surgeon’s discretion, adjunct fixation in the form of screws outside of the plate were used. All retinacular tears were repaired during the standard closure, which was performed in layers.”
Good news overall
“Surprisingly,” said Dr. Shymon, “we found that patella fractures treated with anterior plates had a much lower rate of hardware irritation and subsequent removal. We were interested in investigating whether this really was the case. We were also interested in seeing how these patients did (i.e., Patient Reported Outcome Measures) at one year post-operatively.”
The researchers found that active knee flexion was 131 6 7 degrees. Five patients (28%) reported implant irritation. Only one patient underwent implant removal (transverse screw removal alone). Twelve of the 14 patients (86%) returned to work at 10 6 7 weeks.
Dr. Shymon: “The most interesting result was how well the patellar plating cohort did. We observed no wound complications, infections, nonunions, malunions, or implant failures. Only one patient underwent implant removal for one transverse screw. Patients with patellar plate constructs were allowed to follow accelerated rehab protocols, which resulted in excellent knee range of motion at one year.”
“Anterior tension band plating is a viable option for the treatment of patella fractures with a low incidence of hardware irritation. Patients can also be counseled that they will continue to demonstrate functional deficits up to one year post-operatively.”