Elizabeth Hofheinz, M.P.H., M.Ed.
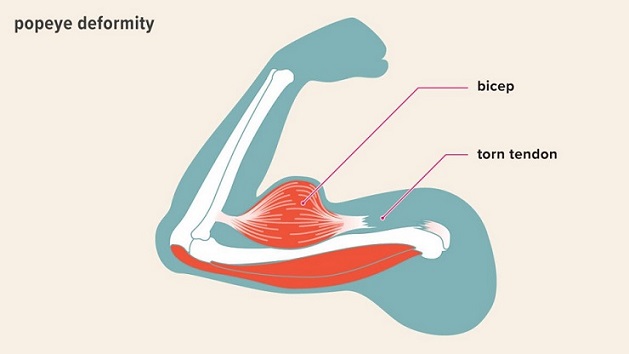
Whether you do a tenotomy or tenodesis for a patient with shoulder pain at the long head of the biceps tendon (LHBT), the results are comparable when it comes to alleviating pain and improving function. But then there is the “Popeye” deformity.
Co-author Moin Khan M.D., M.Sc. is with St. Joseph’s Healthcare Hamilton in Ontario. Dr. Khan told OSN: “Proximal biceps pathology is quite commonly seen, particularly when managing patients with rotator cuff tears. The two most commonly performed procedures to manage this are either a tenotomy of the biceps tendon or a tenodesis. While the tenotomy is technically easier and more commonly performed, we wanted to evaluate the best available evidence – only randomized controlled trials – to see if one of these procedures is actually better than the other one with regards to pain and function as well as cosmetic appearance.” The study, “A meta-analysis of level I evidence comparing tenotomy vs tenodesis in the management of long head of biceps pathology,” appears in the May 2021 edition of the Journal of Shoulder and Elbow Surgery.
The researchers, who searched Ovid Medline, Ovid Embase, and the Cochrane Central Register of Controlled Trials, assessed studies performed from January 1, 1946, to April 17, 2020. Five studies (227 tenotomy and 227 tenodesis patients) met the inclusion for criteria.
Tenodesis: Risk of Popeye Deformity 3X Less
“The most important finding of this research is that although both tenotomy and tenodesis are successful in alleviating pain and improving function, tenodesis significantly reduces the risk of patients developing a bulge of their biceps muscle – which is commonly described as a Popeye deformity. In fact, the risk of developing this deformity is three times less if a tenodesis is performed. These results are important, and surgeons should counsel their patients regarding the risk of Popeye deformity and discuss options for tenotomy and tenodesis at the time of surgery.”
Looking forward, Dr. Khan added: “Further study is needed to assess patient preferences regarding treatment options given the best available evidence – this will help ensure that surgeons counselling patients prior to surgery are aware of patient concerns and potential preferences.”