NEW YORK, Sept. 15, 2021 /PRNewswire/ — Value-based care initiatives can both improve the quality of treatment for patients undergoing orthopedic surgery and reduce overall costs — if the financial incentives for payers and providers are aligned and hospitals have access to key data on utilization of resources and postoperative outcomes.
That’s the conclusion of a new study by researchers at Hospital for Special Surgery (HSS), in New York City, who assessed the clinical and financial effects of such initiatives for its patients undergoing hip and knee replacement surgery. Between 2014 and 2019, implementation at HSS of so-called bundled payment programs for the two procedures saved the Centers for Medicare & Medicaid Services (CMS) nearly $24 million while reducing readmissions and the utilization by patients of costly but at times medically unnecessary postoperative treatments such as intensive rehabilitation.
“Under the BPCI [Bundled Payments for Care Improvement Initiative] and CJR [Comprehensive Care for Joint Replacement] bundle programs, we were able to provide high-quality care efficiently, which in turn led to good outcomes for patients and cost savings for the payer,” said Catherine MacLean, MD, PhD, Chief Value Medical Officer at the HSS Center for the Advancement of Value in Musculoskeletal Care, and the lead author of the study.
The results were published by Dr. MacLean and other HSS colleagues in an article titled “The clinical, operational and financial components of a successful bundled payment program for lower extremity total joint replacement,” which appears in the October issue of NEJM Catalyst Innovations in Care Delivery.
In bundled payment programs, CMS provides a lump sum to physicians and/or hospitals to perform certain procedures, in this case, knee and hip replacement surgery. Doctors and hospitals that provide care at a cost lower than the target amount can keep the savings — so long as certain quality standards are met. However, if the cost is higher, the hospitals must cover the amount above the target price.
The goal of these programs is to push health care providers to develop innovations and efficiencies that save money while preserving, or even improving, the quality of care. Savings can be used by the hospital to develop and deliver additional services that are aimed at improving quality and achieving the best use of health care resources.
As the results reported in the new study suggest, bundled payment programs can work well. However, Dr. MacLean said the success of the bundled care program at HSS — and other medical centers that hope to achieve similar results — hinges on access to the kind of granular data about patient outcomes that CMS provides HSS and other facilities that participate in the agency’s CJR payment model. Under the CJR, HSS is able to track the use of services and Medicare expenditures for individual patients once they leave the hospital, matching them with the hospital’s electronic medical records system. “These data allow us to better understand what happens to our patients once they are discharged and why some are readmitted,” Dr. MacLean said.
One example of an enhancement in care that was enabled by access to granular CJR data involved the identification of a significant number of hip and knee replacement patients who had excessively long stays in skilled nursing facilities after their operations. “It didn’t make sense that patients who walked into a hospital for an elective procedure were staying in a nursing home for 26 days,” Dr. MacLean said.
HSS responded to that information by implementing a health optimization program to identify and tailor care to patients with conditions known to lead to worse postoperative outcomes — such as uncontrolled diabetes and malnutrition. HSS surgeons placed greater emphasis on pre-surgery physical therapy to ensure patients are as fit as possible prior to their operations. In addition, the hospital created clear pathways to help clinicians determine the optimal form of rehabilitation for patients upon discharge.
Although the CJR specifically covers knee and hip replacement patients, Dr. MacLean said the lessons learned from the data have led to wide-ranging benefits. “The programs that we have put in place as a result of our analysis of CJR data have had a spillover effect on how we manage our entire population. As a proof point, our Medicare spending per beneficiary improved from the 62nd to the 16th percentile nationally during the study period,” she said.
Dr. MacLean’s group is now working on an analysis of the effectiveness and efficiencies of HSS@Home, a telemedicine physical therapy program launched in 2018, before the COVID-19 pandemic.
About HSS
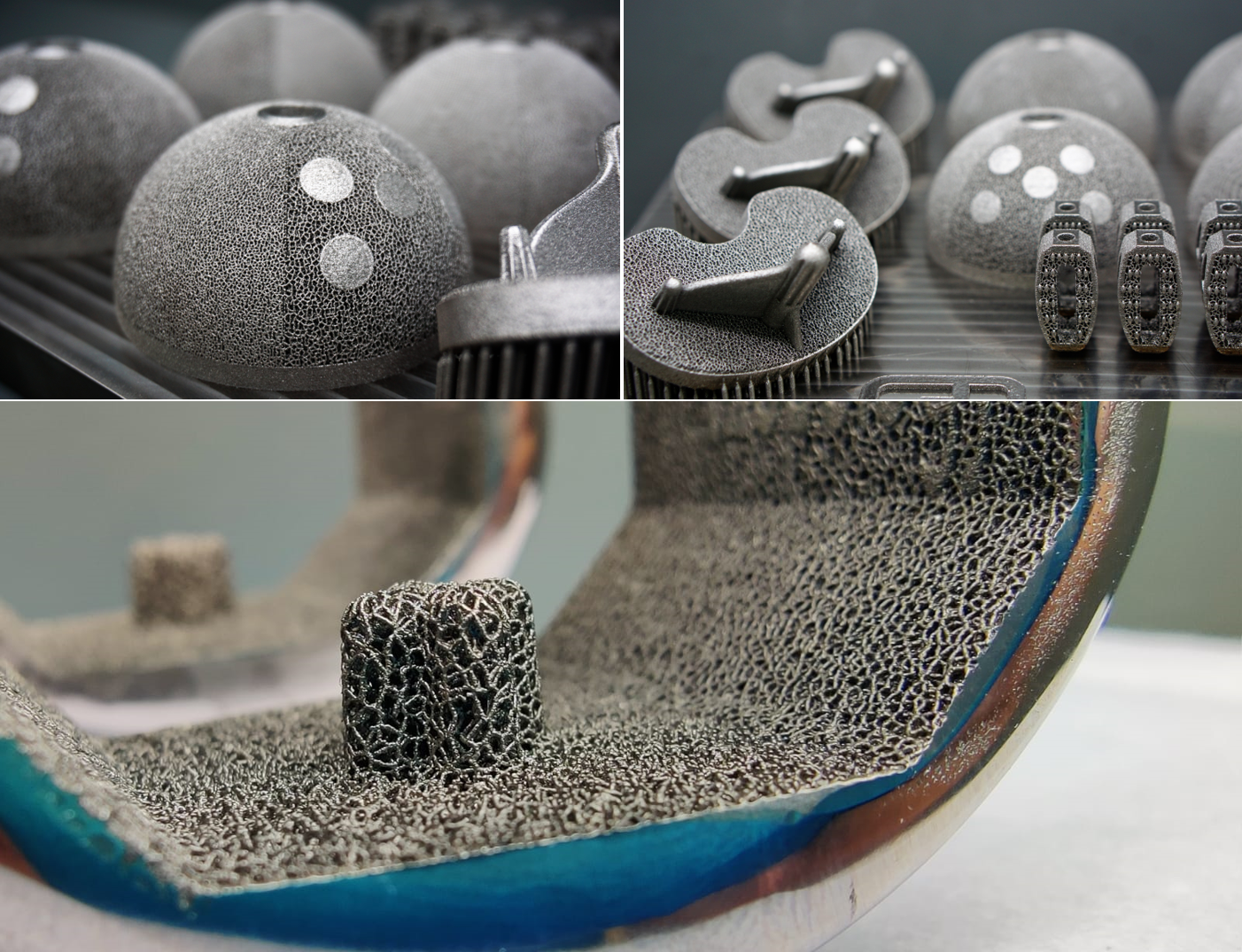
HSS is the world’s leading academic medical center focused on musculoskeletal health. At its core is Hospital for Special Surgery, nationally ranked No. 1 in orthopedics (for the 12th consecutive year), No. 4 in rheumatology by U.S. News & World Report (2021-2022), and the best pediatric orthopedic hospital in NY, NJ and CT by U.S. News & World Report “Best Children’s Hospitals” list (2021-2022). HSS is ranked world #1 in orthopedics by Newsweek (2020-2021). Founded in 1863, the Hospital has the lowest complication and readmission rates in the nation for orthopedics, and among the lowest infection rates. HSS was the first in New York State to receive Magnet Recognition for Excellence in Nursing Service from the American Nurses Credentialing Center five consecutive times. The global standard total knee replacement was developed at HSS in 1969. An affiliate of Weill Cornell Medical College, HSS has a main campus in New York City and facilities in New Jersey, Connecticut and in the Long Island and Westchester County regions of New York State, as well as in Florida. In addition to patient care, HSS leads the field in research, innovation and education. The HSS Research Institute comprises 20 laboratories and 300 staff members focused on leading the advancement of musculoskeletal health through prevention of degeneration, tissue repair and tissue regeneration. The HSS Global Innovation Institute was formed in 2016 to realize the potential of new drugs, therapeutics and devices. The HSS Education Institute is a trusted leader in advancing musculoskeletal knowledge and research for physicians, nurses, allied health professionals, academic trainees, and consumers in more than 130 countries. The institution is collaborating with medical centers and other organizations to advance the quality and value of musculoskeletal care and to make world-class HSS care more widely accessible nationally and internationally. www.hss.edu.
SOURCE Hospital for Special Surgery