First Study to Demonstrate Longer-Term Benefits of Modern Hip Arthroscopy Techniques
NEW YORK, April 18, 2024 /PRNewswire/ — A new study by surgeon-scientists at Hospital for Special Surgery (HSS) found that 25% of patients with hip impingement who underwent modern arthroscopy for their condition experienced a delay in the natural progression of osteoarthritis. The retrospective study, published online on March 8, 2024, in The American Journal of Sports Medicine, is the first to link hip arthroscopy with a reduced risk of developing hip arthritis over the long term.
“I’m very proud of our team for publishing this work, which validates hip arthroscopy as a longer-term joint-preserving procedure in carefully selected patients,” says Bryan T. Kelly, MD, MBA, President and CEO of HSS and a world-renowned pioneer in the field of hip arthroscopy who also served as senior author on the study. “At HSS, we focus on providing excellence in clinical care through innovation and evidence-based research. This paper is a prime example of the benefits of advancing innovations in surgical techniques and analyzing patient data collected over many years so we can understand and share the factors associated with optimal results.”
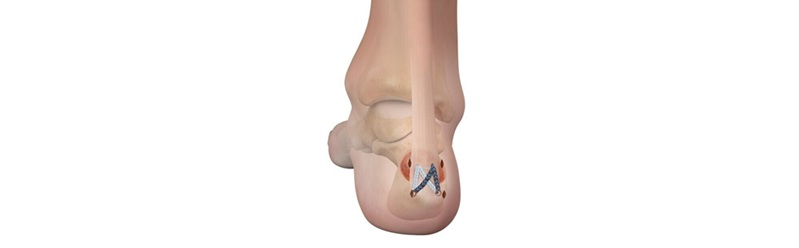
Hip impingement, also called femoroacetabular impingement (FAI), is a condition that typically arises between the teenage years and middle age, and is the underlying cause of hip pain in about 40% of patients in this age range. Hip impingement occurs when the bones of the hip joint are not shaped properly, causing them to rub against one another. Over time, the persistent friction can lead to pain and stiffness, eventually progressing to advanced arthritis.
Prior studies have shown that 85-90% of patients with hip impingement who undergo modern arthroscopy return to their usual activity level. However, until now, little has been known about whether modern arthroscopy can slow the progression of arthritis in these patients. To explore this connection, investigators examined X-ray images of 200 hips from 100 patients who exhibited signs of impingement in both hips but only underwent arthroscopy for their symptomatic hip between 2010 and 2012. The severity of arthritis in each hip was assessed retrospectively using X-ray images taken before surgery and at least 10 years later. Notably, the researchers were unaware of which hips had undergone surgical correction during the assessment.
The resulting analysis revealed only 28% of operative hips showed an increase in arthritis progression at a minimum of 10 years after surgery in comparison to 48% of nonoperative hips. This difference translated to a relative risk reduction of 42% across all patients.
While there was no difference in the natural development of arthritis between the operative and nonoperative hips for 70% of patients, one in four, or 25%, had less arthritis in their operative hip compared to their nonoperative hip 10 years later.
“Previous studies by other centers have reported underwhelming 10-year arthroplasty outcomes for patients with hip impingement. However, those studies reported on older surgical indications and older surgical techniques,” explains lead author and former HSS fellow Prem N. Ramkumar, MD, MBA, now an orthopedic surgeon at Long Beach Lakewood Orthopedic Institute, in Long Beach, California. “By contrast, we studied the effect of modern arthroscopic methods by comparing the degree of arthritis in each patient’s operative hip versus their nonoperative hip. Our research design controlled for variables such as age, medical history, lifestyle, and individual mechanics like rotational profile, spinal alignment and gait—leaving history of arthroscopy as the single factor driving any resulting differences in arthritis progression.”
In addition, the investigators identified a small subset of patients whose arthritis progressed more rapidly in the operative hip as compared to the nonoperative hip. Specifically, older age, a higher arthritis grade, an alpha angle greater than 65 degrees and evidence of borderline hip dysplasia before surgery were the primary risk factors associated with the 5% of hip impingement patients whose arthritis in the operative hip worsened more quickly after surgery.
“We can now identify patients most likely to benefit from arthroscopy for hip impingement and inform patients about their anticipated odds of successful outcomes based on their personal risk factors. For ideal candidates, the evidence shows that hip arthroscopy may delay or prevent arthritis for one in four patients. That’s very powerful information,” says Danyal W. Nawabi, MD, FRCS, an HSS orthopedic surgeon and an author on the study.
Dr. Nawabi also points to the importance of the modern techniques used to care for patients in the study, all of whom were patients of Dr. Kelly. These methods include labrum repair, removal of bony abnormalities on the ball and socket, and proper closure of the joint capsule enveloping the hip joint. “This study is a testament to the fact that where you go for orthopedic care truly matters,” he adds.
Thus far, the paper has garnered two awards: the 2024 American Orthopedic Society for Sports Medicine Fellow Research Award for Clinical Science, which will be presented at the AOSSM Annual Meeting in July, as well as the Philip D. Wilson, MD, Award, presented by HSS in honor of the hospital’s fifth Surgeon-in-Chief to a fellow who has demonstrated excellence in orthopedic surgery research.
About HSS
HSS is the world’s leading academic medical center focused on musculoskeletal health. At its core is Hospital for Special Surgery, nationally ranked No. 1 in orthopedics (for the 14th consecutive year), No. 2 in rheumatology by U.S. News & World Report (2023-2024), and the best pediatric orthopedic hospital in NY, NJ and CT by U.S. News & World Report “Best Children’s Hospitals” list (2023-2024). In a survey of medical professionals in more than 20 countries by Newsweek, HSS is ranked world #1 in orthopedics for a fourth consecutive year (2023). Founded in 1863, the Hospital has the lowest readmission rates in the nation for orthopedics, and among the lowest infection and complication rates. HSS was the first in New York State to receive Magnet Recognition for Excellence in Nursing Service from the American Nurses Credentialing Center five consecutive times. An affiliate of Weill Cornell Medical College, HSS has a main campus in New York City and facilities in New Jersey, Connecticut and in the Long Island and Westchester County regions of New York State, as well as in Florida. In addition to patient care, HSS leads the field in research, innovation and education. The HSS Research Institute comprises 20 laboratories and 300 staff members focused on leading the advancement of musculoskeletal health through prevention of degeneration, tissue repair and tissue regeneration. In addition, more than 200 HSS clinical investigators are working to improve patient outcomes through better ways to prevent, diagnose, and treat orthopedic, rheumatic and musculoskeletal diseases. The HSS Innovation Institute works to realize the potential of new drugs, therapeutics and devices. The HSS Education Institute is a trusted leader in advancing musculoskeletal knowledge and research for physicians, nurses, allied health professionals, academic trainees, and consumers in more than 165 countries. The institution is collaborating with medical centers and other organizations to advance the quality and value of musculoskeletal care and to make world-class HSS care more widely accessible nationally and internationally. www.hss.edu.
SOURCE Hospital for Special Surgery