Robotics and navigation systems have the potential to drastically change how surgical procedures are conducted across the country, offering greater precision, faster recovery times and new possibilities for complex procedures.
As this technology evolves, providers face critical decisions such as how to invest wisely, train staff and integrate robotics into existing surgical workflows.
In this episode, Brent Ford, senior clinical director of medical device management at HealthTrust Performance Group, and Dr. Michael Gallizzi, a leading spine surgeon at the Steadman Clinic, discuss the impact of robotics and navigation systems on healthcare organizations and patient care.
Our featured experts discuss the costs, benefits and challenges hospitals should consider, share success stories from the field, and look ahead to where surgical robotics may go in the future.
Transcript
Maria Castellucci:
Hello and welcome to Healthcare Insider, a sponsored content podcast series from Modern Healthcare Custom Media. I’m your host, Maria Castellucci, deputy editor of custom content at Modern Healthcare. It’s my pleasure to welcome to the podcast Brent Ford and Dr. Michael Michael Gallizzi. Brent is senior Clinical Director of Medical Device Management at HealthTrust Performance Group, and Dr. Michael Gallizzi is a spine surgeon at the Steadman Clinic based in Vail, Colorado. Thank you both so much for being here today. I’m really looking forward to our conversation.
Dr. Michael Gallizzi:
Yeah, thank you Maria. Very nice to speak with you today.
Maria Castellucci:
So our conversation today will be about the business considerations hospitals and health systems should make as they weigh investments in surgical robotics and navigation systems. So Brent, I’d love to start with you. Can you talk through the current state of the surgical robotics and navigation systems industry specifically, can you share how commonplace these devices are? Do we expect the space to grow? Who are the big players in the market? Please just kind of give us an overview.
Brent Ford:
For the last couple decades, this type of technology in spine surgery specifically has been limited to navigation. Only The market really has evolved to include many things, preoperative planning tools, enhanced imaging, robotics, augmented reality, and endoscopic spine surgery. I would think enabling tech is really so common now that if you don’t have an option, you might be at a disadvantage as a vendor. The market, it’s had a steady growth and some spurts with some drawbacks being higher cost and slower adoption. I think from the field, and I think Dr. Zi would probably agree there. The other factor I look at is how quickly the technology is dated and replaced by second generation technology, very similar to our electronics world that we live in. So all all I think the global surgical robotics market really is expected to grow probably around 9% is what the forecasted rate is within the next six years. And I think some of the leaders in the market right now, the leaders that we see are globalist medical and Medtronic for the robotic market. Some very promising technologies that we’ve seen are technologies like on point surgicals, augmented reality platform, and a GDA medicals predictive analytics system.
Maria Castellucci:
Thank you so much for that Really great overview of the market overall. I’d like to then narrow in a little bit with Dr. Gallizzi here. Dr. Gallizzi, can you share how you’re using robotics and navigation in your practice today? Which procedures do you leverage robotics and navigation in the most? And then are you performing spinal fusions with a robot?
Dr. Michael Gallizzi:
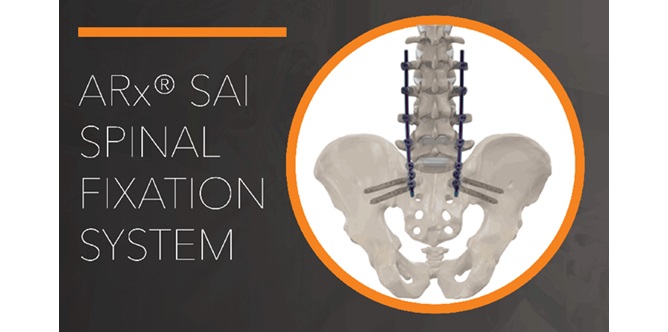
Yeah, absolutely, and I agree with Brent that those are some of the market leaders, especially I know more about the spine market as opposed to let’s say the total joint market, which I know has seen a huge growth as well. For me, I started using robotics in my practice. I was sort of an earlier adopter in 2019. I was the first globus robotic user in the state of Colorado and subsequently have nearly approached 400 cases during that time. And so as I evolved originally it was a really great tool for me as a physician, especially someone who’s a cancer survivor, to decrease the amount of radiation in my or to my staff and to everyone around me. And that was sort of the original big draw that in the increased precision that it affords. And so I was originally trained to do percutaneous pedicle screws under fluoro and obviously if you’re taking a bunch of small x-rays repetitively that repetitive dose over many, many screws over many, many years that radiation dose adds up. And after sort of the piece that I went through personally, that really helped drive my adoption to be able to say, Hey, how can I use an enabling technology to do what I’m doing now in a safer, more reproducible way so that I can have a longer career and spare some radiation to all my colleagues around me. And so originally it was just putting in placing screws and the globus platform at that time did not have an imaging device with it. And so we would pair it either with a preoperative CT scan or sometimes we would use the Medtronic O arm to be our preoperative CT scan and that would upload the patient’s imaging to the robotic planning software. And like Brent mentioned before, that planning software really started to increase in the fidelity of exactly how long a screw the location of the screw lining up the screws and then avoiding facet joint violations, cran and coddly and having more precise location to be able to line them up because all my screw placement is really percutaneous. So with that, I started learning that the robotic system and the planning software as opposed to a navigation only software at that time really allowed me to plan a construct and not just one screw at a time. So what do I mean by that? That’s if I’m placing six screws or even doing an L two to pelvis, I’m able to line up all those screw heads in the right location to easily or more easily be able to pass a rod in the subcutaneous tissue and connect and hit all my marks. And so what it really added to me was that ability, again, to plan the entire surgery, not just surgery by itself. Then as the software as Brent alluded to, sometimes the tech, you outgrow the tech and you want a new iPhone and you want the bigger TV and all the new fangled things. Well, the nice thing was with the platform that I use is they did the software updates to enhance that and they didn’t have to necessarily change the hardware. There have been some additional hardware things that have been added like interbody solutions where you’re able to navigate actual inner bodies that are placed in between the vertebral bodies, T lift cages or lateral cages in order to again decrease radiation and add that surgical planning element to the case itself. And over time I started increasing the use of the robot. So I started saying, okay, this robotic system and planning software really lets me target whatever I want. So if a patient had difficult deep hardware, a case comes to mind like a SI joint fusion that was performed and unfortunately one of those SI joint fusion screws was placed too deep into the patient and into the neuro foramen. And what that spurred me to do is actually be able to use the robot to plan over that previous hardware and actually do a small dissection right down to that hardware. And then what I encountered was a bunch of scar tissue I couldn’t get the screwdriver in. So then at that time I was like just endoscopic spine surgery was also growing and I was like, Hey guys, just grab the endoscope. So then I actually put the endoscope through the robot targeted the tissue that was overgrowing on that was able to debride that tissue off and then easily get that screwdriver in. So instead of just flailing in that patient’s body trying to get the screwdriver in and scrape stuff off and creating this all collateral damage, I was able to really use all the enabling technology I had at the time to precisely do that. And it took something that would probably have taken two and a half hours and all of a sudden we were done in 45 minutes. So that sort of progressed to revision cases where there’s a huge block of bone placed in the posterior lateral space and they didn’t quite decompress that nerve. And so when they had sustained radiculopathy and that nerve was continued to be compressed, I was able to plan small little screw trajectories just in the bone and I was able to essentially make a small little planned divot hole in a clover leaf pattern almost all the way down to the neural elements, but not to them, but pretty close to them, and then bring in a microscope, finish it off by hand, and just by being able to drill down confidently through an abnormal anatomy or block of bone to be able to get there precisely and efficiently, that’s how I started using the robot. And it excelled to placing percutaneous pedicle screws in the cervical spine, which is a new addition that just came out a couple of weeks ago. And also placing pars screws for young adolescent athletes who have a pars fracture that’s fresh and we’re able to actually just drill that, throw a compression screw across that in a wire and then efficiently take care of that very precisely minimally invasively and taking more complex cases and being able to get that planning done to be able to perform them efficiently and with the least amount of soft tissue damages possible.