June 23, 2025, Author: Thomas L. Bernasek, MD –
Recent Trends in Total Hip Arthroplasty
Recognized as the “operation of the century”, total hip replacement (THR) has helped millions of patients overcome pain and return to normal activity. 1 Despite this, continuous analysis of THR is necessary to further improve surgical technique and to decrease complications and adverse outcomes. In recent years, several trends have emerged in the field of Total Hip Arthroplasty (THA), reflecting the continuous pursuit of improving surgical outcomes and patient satisfaction. One notable trend is the shift to improve surgical techniques. Modern surgical approaches aim to reduce tissue damage, minimize scarring, and accelerate recovery times. By utilizing smaller incisions and specialized instruments, surgeons can perform THA with greater precision and less disruption to surrounding tissues, enhancing the overall patient experience.
The integration of digital technologies and data analytics is transforming the landscape of THA. Surgeons now have access to sophisticated software that aids in preoperative planning and intraoperative navigation. These tools provide real-time feedback and enhance surgical precision, contributing to improved implant positioning and alignment. As we continue to embrace these technological advancements, the future of THA looks promising, with the potential to further optimize patient outcomes and redefine the standards of care.
Innovations in Surgical Techniques
Innovations in surgical techniques have played a pivotal role in advancing THA, offering patients safer and more effective treatment options. One of the most significant developments is the adoption of the direct anterior approach (DAA). Unlike traditional approaches that involve detaching muscles, the DAA allows surgeons to access the hip joint by navigating between muscle planes. This muscle-sparing technique results in less postoperative pain, faster recovery, and improved joint function. This allows many THA procedures to be performed on an outpatient basis.
Another innovative technique gaining traction is computer-assisted surgery (CAS). CAS leverages advanced imaging and navigation systems to guide surgeons during the procedure, ensuring precise implant placement and alignment. This technology enhances the surgeon’s ability to achieve optimal implant alignment, reducing the risk of complications such as dislocation and implant loosening. As a proponent of evidence-based practice, I have witnessed the positive impact of modern THA on patient outcomes, with many patients experiencing quicker rehabilitation and longer-lasting results.
Additionally, robotic-assisted surgery is making waves in the field of hip arthroplasty. Robotic systems offer unparalleled precision and control, allowing surgeons to perform complex procedures with enhanced accuracy. By utilizing preoperative imaging and real-time feedback, robotic-assisted surgery ensures that implants are positioned with exceptional precision, reducing the likelihood of human error. This innovative approach not only improves surgical results but also boosts patient confidence in the procedure’s success.
Advances in Prosthetic Materials
The evolution of prosthetic materials has been instrumental in enhancing the durability and longevity of hip implants. One of the most significant advancements is the development of highly cross-linked polyethylene (HXLPE). This material exhibits superior wear resistance compared to traditional polyethylene, reducing the risk of osteolysis and implant loosening. As a result, HXLPE has become the gold standard for the acetabular component of hip implants, offering patients improved long-term outcomes.
Another noteworthy innovation is the use of ceramic-on-ceramic and ceramic-on-polyethylene bearings. Ceramic materials are known for their exceptional hardness, low friction and biocompatibility, resulting in reduced wear. These properties make ceramic bearings an attractive option for younger, more active patients who require implants with extended longevity. As a surgeon, I have observed the benefits of ceramics and highly cross-linked polyethylene materials in minimizing wear-related complications and enhancing the overall success of THA.
The introduction of porous metal coatings has revolutionized the fixation of hip implants. These coatings promote osseointegration, allowing the bone to grow into the implant and achieve stable fixation without the need for cement. This advancement has significantly improved the outcomes of cementless hip arthroplasty, offering patients a more natural and durable solution. As we continue to explore new materials and surface technologies, the future of prosthetic design holds promise for even greater advancements in THA.
Impact of Robotics and AI in Hip Arthroplasty
The integration of robotics and artificial intelligence (AI) in hip arthroplasty represents a paradigm shift in surgical practice, offering unprecedented levels of precision and customization. Robotic-assisted surgery, as previously mentioned, provides surgeons with enhanced control and accuracy, ensuring optimal implant positioning and alignment. This technology is particularly beneficial in complex cases where precise measurements and adjustments are crucial for achieving successful outcomes.
AI, on the other hand, is revolutionizing preoperative planning and decision-making in THA. Machine learning algorithms can analyze vast amounts of patient data to predict potential complications and tailor surgical strategies accordingly. This data-driven approach allows surgeons to identify high-risk patients and implement preventive measures, improving patient safety and outcomes. As an advocate for leveraging technology in healthcare, I believe that the integration of AI in THA has the potential to redefine personalized medicine and enhance patient care.
Moreover, robotics and AI are facilitating advancements in postoperative rehabilitation and monitoring. Wearable devices equipped with sensors can track patients’ progress and provide valuable insights into their recovery journey. These devices enable remote monitoring and timely interventions, ensuring that patients receive the support they need to achieve optimal outcomes. As we continue to harness the power of robotics and AI, the future of hip arthroplasty holds promise for more efficient, patient-centered care.
The Reverse Hip Replacement System
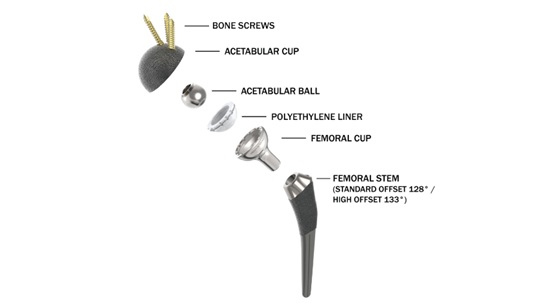
The Reverse Hip Replacement System (HRS) represents a significant advancement in hip replacement technology. This innovative Metal-on-Polyethylene reverse geometry hip prosthesis differs from conventional systems by positioning the ball within the acetabular cup instead of the femoral stem. Currently undergoing FDA-monitored clinical trials, the Reverse HRS has demonstrated promising results through extensive testing in over 90 pre-clinical experiments. This system aims to enhance stability during extended ranges of motion while reducing dislocation risks, particularly benefiting patients with complex hip conditions. THR instability and dislocation remains a significant possible complication and is more likely in patients with spinal fusion and certain surgical approaches. The reverse hip hold promise as it addresses this problem by allowing increased range of motion without impingement or dislocation.
The exceptional stability of the Reverse HRS derives from its unique component interaction. As the hip undergoes flexion-extension, abduction-adduction, and internal-external rotation, the femoral cup overlaps and articulates with the acetabular cup. This interlocking mechanism significantly reduces impingement and dislocation risk. Clinical testing has demonstrated that dislocation with the Reverse HRS requires both traction and laterally directed force in neutral position — a combination rarely occurring in normal movement patterns.

Figure 1: The current Reverse HRS Product Family includes Standard and High offset component devices.
Patient Outcomes and Satisfaction
Enhancing patient outcomes and satisfaction is the ultimate goal of THA. With the advancements discussed earlier, patients undergoing THA today can expect improved functional outcomes, reduced pain, and quicker recovery times. The shift towards improved surgical techniques and personalized implants has significantly contributed to these positive outcomes, enabling patients to resume their daily activities with renewed confidence.
Patient satisfaction is also influenced by the level of engagement and communication throughout the surgical journey. As a healthcare provider, I prioritize open communication with my patients, ensuring they are well-informed about the procedure, potential risks, and expected results. This approach fosters trust and empowers patients to actively participate in their recovery process.
The success of THA is measured not only by clinical outcomes but also by patients’ perceived quality of life. By continuously refining surgical techniques and embracing technological innovations, we can offer patients a more satisfying and fulfilling experience, helping them regain their independence and enjoy a higher quality of life.
Challenges and Future Directions
Despite the remarkable advancements in THA, several challenges remain that warrant attention. One of the primary challenges is the management of postoperative complications, such as infection and implant failure. While the rate of these complications has decreased significantly over the years, they still pose a risk to patient outcomes. Continued research and innovation are needed to develop strategies for early detection and effective management of these complications.
Another challenge lies in addressing the needs of an aging population. As the demand for hip arthroplasty continues to rise, healthcare systems must adapt to accommodate the growing number of patients requiring joint replacement surgery. This includes optimizing surgical workflows, streamlining rehabilitation programs, and ensuring access to high-quality care for all patients. As a healthcare provider, I am committed to advocating for policies and practices that prioritize patient-centered care and equitable access to THA.
Looking ahead, the future of THA holds promise for further advancements in surgical techniques, prosthetic materials, and patient care. The integration of regenerative medicine, such as stem cell therapy and tissue engineering, has the potential to revolutionize joint replacement surgery by promoting natural healing and tissue regeneration. As we continue to explore these innovative approaches, we can look forward to a future where THA offers even greater benefits to patients worldwide.
Conclusion
THA has steadily improved since its inception, evolving into a highly effective and reliable solution for individuals suffering from hip joint damage. The recent trends and innovations in surgical techniques, prosthetic materials, and digital technologies have significantly enhanced patient outcomes and satisfaction, offering a brighter future for those in need of hip replacement surgery.
As an orthopedic professional, I am committed to staying informed about the latest advancements in THA and incorporating them into my practice to provide the best possible care for my patients. By embracing innovation and prioritizing patient-centered care, we can continue to improve the quality of life for individuals undergoing THA.
For those considering hip replacement surgery, I encourage you to consult with a qualified orthopedic surgeon to explore your options and determine the best approach for your unique needs.

Thomas L. Bernasek, MD, is fellowship-trained in adult reconstruction hip and knee replacement. Prior to becoming a founding member of Florida Orthopaedic Institute, Dr. Bernasek received his medical training at the Creighton University College of Medicine in Omaha, Nebraska, and completed his Orthopedic Residency training at the University of New Mexico. After residency, Dr. Bernasek completed a fellowship in joint replacement and adult reconstruction at the Mayo Clinic in Rochester, Minnesota.
He is known nationally and internationally as an expert in joint replacement with vast experience in total hip and knee replacement. His articles have been published in numerous professional journals, and he has presented research papers and lectured at medical conferences on the national and international level for over three decades. He maintains active involvement in numerous orthopedic research and development projects and is a professor in Orthopaedic surgery at the University of South Florida College of Medicine. Dr. Bernasek is the director of the Florida Orthopaedic Institute Adult Reconstruction Fellowship, a trustee of the Florida Orthopedic Society, a trustee of the Foundation for Orthopeadic Research and Education and a past president of the Hillsborough County Medical Association.
1. Lancet. 2007 Oct 27;370(9597):1508-19. doi: 10.1016/S0140-6736(07)60457-7.
The operation of the century: total hip replacement