Morgan P. Lorio and Kai-Uwe Lewandrowski
International Journal of Spine Surgery, January 2026, 8848; DOI: https://doi.org/10.14444/8848
A Profession in Free Fall
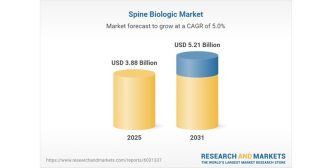
Over the past 20 years, the work of spine surgeons has been systematically devalued. Adjusted for inflation, Medicare reimbursement for the 15 most common spinal procedures has fallen 33.8% since 2000—an average loss of nearly 2% per year.1 No cost-of-living adjustment (COLA) has been applied to the Physician Fee Schedule since 2001, while practice expenses have climbed by more than 60%.
The arithmetic of “budget neutrality” ensures redistribution rather than growth: when one code rises, another falls. The rhetoric of value-based care masks an economy of attrition—surgeons are told to do more, faster, for less, in the name of quality. The median-quartile valuation method embedded in the Relative Value Scale Update Committee (RUC) process guarantees that “reasonable and customary” work is reimbursed at the bottom quartile of its worth. What is being sold as efficiency is often just attrition with better branding. The result is not sustainability; it is exhaustion (Figure 1).
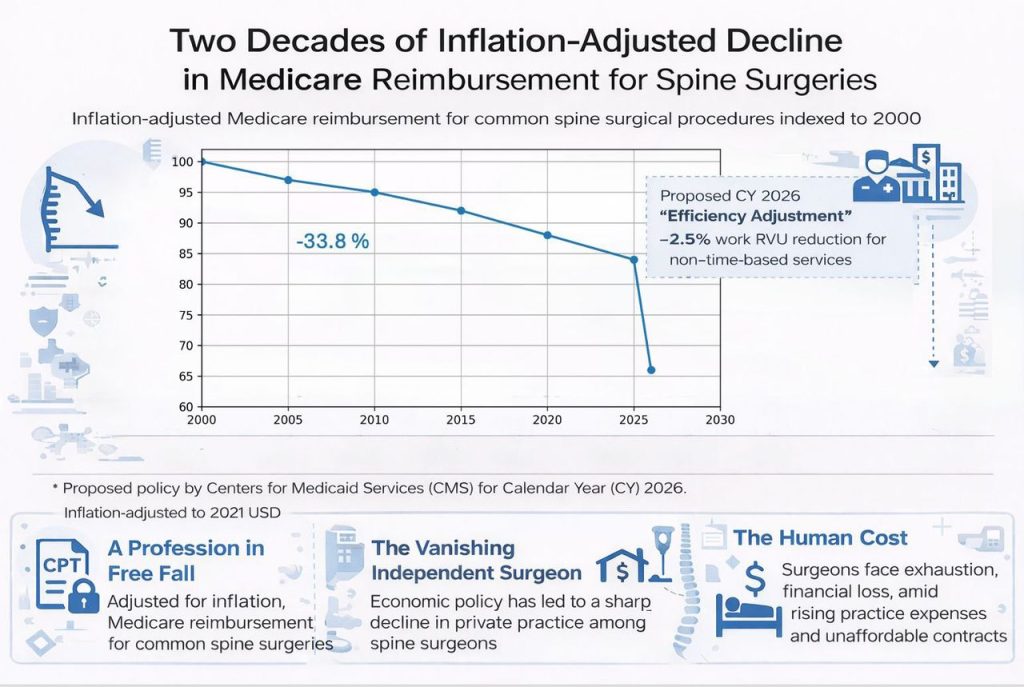
Figure 1
Inflation-adjusted Medicare reimbursement for common spine surgical procedures indexed to 2000, illustrating a 33.8% decline since 2000 and highlighting the proposed CY 2026 Centers for Medicaid Services (CMS) “efficiency adjustment” (−2.5% work Relative Value Unit [RVU], nontime-based services). Surrounding panels summarize linked consequences: declining independent practice, Current Procedural Terminology/Relative Value Scale Update Committee (RUC) valuation concerns, and surgeon burnout/financial strain.
A particularly revealing manifestation of this erosion is the Centers for Medicare & Medicaid Services (CMS’s) proposed 2026 “efficiency adjustment,” which applies a 2.5% reduction to work RVUs for non–time-based procedures. This marks a decisive break from the long-standing RUC construct defining physician work as the product of time and intensity. In its place, CMS substitutes assumed efficiency gains derived from administrative logic rather than observed clinical practice. In spine surgery, this assumption is demonstrably false. Operative times are not contracting; they are expanding as patient age, comorbidity burden, and procedural complexity increase—especially with minimally invasive techniques that demand higher cognitive load, technical precision, and intraoperative judgment. By presuming efficiency where none exists, policy quietly devalues surgical labor while preserving the façade of budget neutrality. What makes this erosion particularly dangerous is that it no longer requires an active decision-maker. A vise grip requires someone to keep turning the screw. A pressure cooker tightens itself. Once assumption replaces observation, the system applies downward pressure automatically—silently, continuously, and without accountability.2
The Vanishing Independent Surgeon
Economic policy has translated directly into sociological change. According to the American Medical Association’s (AMA’s) 2023 Physician Practice Benchmark Survey, only 46.7% of physicians now work in private practice, and just 44% are self-employed. Among physicians younger than 45 years, self-employment has collapsed to 31.7%.3
Eighty percent of physicians who sold their practices to hospitals cited the same reason: they could no longer negotiate fair rates or manage the administrative burden alone. Physicians did not abandon independence; policy made independence mathematically impossible. What was once a profession of accountable professionals has been transformed into shift work inside corporate medicine.
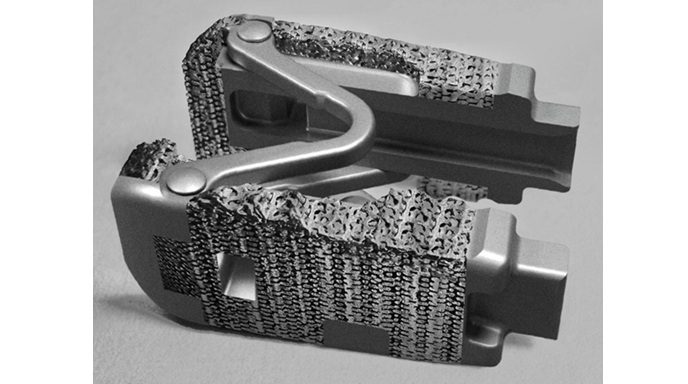
The Codified Monopoly
When Senator Bill Cassidy, MD, wrote to the AMA in 2025, his concern was not partisan but structural: how a privately owned and trademarked code set could function as a government-mandated standard for the transaction of medical care. Under Health Insurance Portability and Accountability Act, Current Procedural Terminology (CPT) is designated a standard medical data code set in federal regulation (45 CFR §162.1002).4 What began as a language of communication now operates as an instrument of governance.5
Senator Cassidy’s inquiry converted long-standing clinician concerns into a formal congressional oversight action. His letter sought transparency regarding CPT governance, the incorporation of nonmember physician input, and the scale of CPT-derived revenue. Reported AMA revenues exceeded $513 million, with $281 million attributed to books and digital content, including coding productsand licensed data files.6,7 When a proprietary language is embedded as mandatory infrastructure—and its steward participates in valuation—the appearance of budget neutrality can mask a systematic transfer of value away from bedside labor and professional judgment (Figure 2).
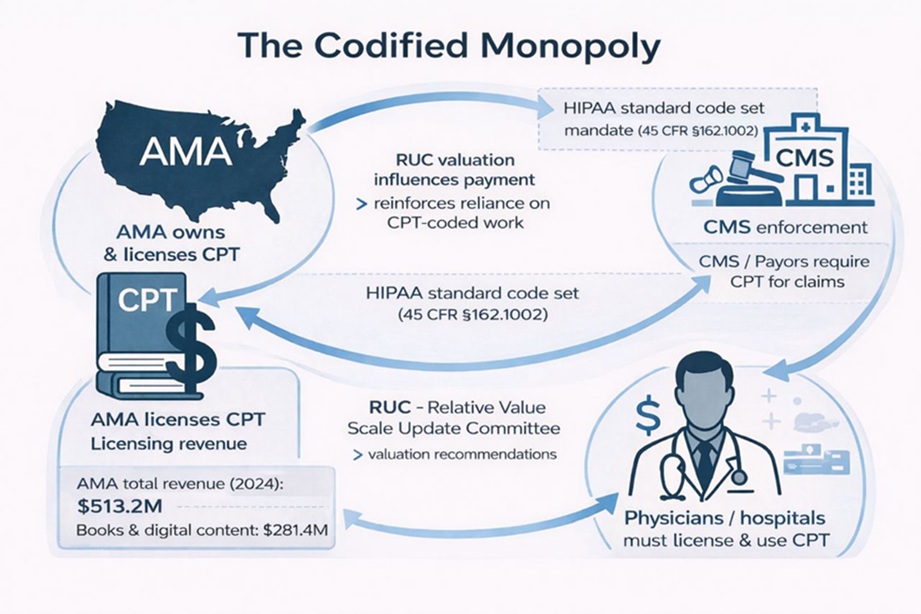
Figure 2
Schematic representation of the Current Procedural Terminology (CPT) governance and valuation ecosystem. The American Medical Association (AMA) owns and licenses the CPT code set; valuation recommendations are developed through the RUC (Relative Value Scale Update Committee); and the Centers for Medical & Medicaid Services (CMS) enforces CPT use for claims through federal rulemaking under Health Insurance Portability and Accountability Act (HIPAA) designation. The circular flow illustrates how mandatory reliance on a proprietary code set, combined with valuation influence and licensing revenue, creates a self-reinforcing system that governs physician work valuation and payment.
CPT no longer functions merely as a professional language; once it became mandatory infrastructure, it became part of the rule book—and rule books with compulsory force require transparency and oversight.
The Human Cost
This article is not written as an abstract policy exercise. It is written from the first author’s perspective as a surgeon who survived COVID-19, a coma, and prolonged convalescence at age 63. That experience stripped away any illusion that resilience alone can outlast structural decay. When I awoke, the profession I loved had changed: physicians were employees, not advocates; codes and conversion factors dictated worth; autonomy had become a memory.
Burnout is often described as emotional fatigue, but that framing is incomplete. It is also economic, moral, and physical. Surgeons now carry among the highest mortality risks of any physician group—a reality that is not coincidental, but cumulative. When professional judgment is stripped of value, autonomy is replaced by compliance, and when meaning is displaced by metrics, the cost is borne not only in exits from practice, but also in lives shortened under sustained moral injury.8,9
There is no way to undo what the virus did, but there may still be a way to undo what policy has done—if we are willing to name it plainly. What began as emergency coordination during the pandemic hardened into economic choreography, binding physicians and patients alike within systems optimized for compliance rather than creativity.6 Kicking the can has been the strategy, and it is time that someone other than the surgeon pays the piper.
The Unaffordable Contract
For many surgeons, participation in federal insurance programs has become a moral conflict disguised as an economic one. Practice expenses—staff, malpractice, rent, and compliance—now routinely outpace reimbursement. Under budget neutrality, even commercial contracts are indexed to depressed public benchmarks. Surgeons cannot afford to accept Medicare or Medicaid without subsidizing care from their own margins. The resulting exodus is quiet, not ideological. It is driven by insolvency.
The Patient’s Parallel Illusion
Patients experience a parallel dissonance. Insurance coverage exists, yet access is rationed through delay, denial, and administrative friction. Patients possess insurance but not care; physicians possess licenses but not autonomy.
“Protection” in modern health care is not safety in the lived sense; it is administrative shelter. It is written as coverage, authorization, guideline adherence, and quality metrics. It sounds like care, but it functions as distance. Someone else defines the threat, the remedy, and the acceptable risk—using a vocabulary the protected party did not create and cannot fully contest.
For patients, protection becomes prior authorization, formularies, step therapy—mechanisms ostensibly designed to prevent harm but often function to delay or dilute care while shielding payers from cost. For professionals, protection becomes compliance. Judgment is replaced by protocol; autonomy is traded for the illusion of security. Follow the rules and you will be safe—until the rules change without warning.
In both cases, protection is externalized. It is not something one possesses; it is something one is allowed to borrow. Because it is written in someone else’s language, it cannot fully name what is actually at risk: dignity, vocation, trust, time, and moral agency. Those losses do not appear in policy text, and so they are treated as acceptable collateral.
The Tea Leaves
Two decades of reimbursement cuts, consolidation, and administrative creep have not accidentally reshaped medicine; they have intentionally done so. Independence has been rendered economically unsustainable. This is controlled by design—economic, regulatory, and cultural. If nothing changes, the next generation will inherit a profession without ownership, creativity, or dissent.
The Illusion of the Fixed Pie
Budget neutrality presumes a fixed physician-payment pie even as national spending expands elsewhere. This is accounting, not truth. As satellite “nightlights” revealed economic activity invisible to Gross Domestic Product (GDP) accounting, so too does clinical labor exceed what reimbursement spreadsheets capture.10 Budget neutrality is to physicians what manipulated GDP is to citizens: a managed illusion of scarcity used to justify inequity.
What a Revolution Would Mean
Revolution need not be reckless. It can be an act of reclamation. It begins when surgeons and other physicians demand reforms that restore coherence between work, value, and care delivery.
First, transparency must be non-negotiable. RUC deliberations, methodology, and voting records should be publicly available so that valuation reflects observed clinical reality rather than opaque consensus.
Second, valuation itself must be reclaimed. Work RVUs should be indexed to the mean, not the bottom quartile, and must rise with a true COLA. In the absence of COLA, inflation is converted into an automatic pay cut, guaranteeing progressive devaluation regardless of productivity or quality.
Third, modernize the Geographic Practice Cost Index (GPCI) by paying physicians the same for the same work, regardless of geography. If we did that, we would stop driving talent away from underserved areas. Instead, the current system penalizes geography—and then acts surprised when access disappears. But geographic equity alone is insufficient if the value of the RVU itself continues to erode. Physician work must increase with a true COLA; otherwise, GPCI merely redistributes a loss rather than preserving the value of care.
Fourth, physicians must be empowered to form surgeon-led collectives that negotiate directly with employers and payers, assume limited and appropriate risk, and retain ownership of outcomes data—particularly the data used to value their work. Independence does not require isolation; it requires leverage aligned with accountability.
Finally, professional autonomy must be recognized as a quality metric. Care is never optimal when physicians are interchangeable labor. Judgment, continuity, and moral agency are not inefficiencies—they are the substrate of safe, humane medicine.
Physicians Are Not Interchangeable Labor
Care is never optimal when physicians are treated as interchangeable labor. Continuity, moral agency, and professional memory define quality care. When physicians are reduced to productivity units, systems may gain efficiency but lose wisdom. Rome did not collapse from lack of manpower; it collapsed when experience was replaced with cheaper substitutes. The patient’s body is not an assembly line, and the surgeon’s judgment cannot be replaced by protocol.
The Vacuum and Its Substitutes
Physician attrition is accelerating. A 2025 Annals of Internal Medicine analysis found clinical-practice attrition rising from 3.5% in 2013 to 4.9% in 2019 across every specialty and region.11 Mid-career exits remove not only capacity but also mentorship and judgment.
Into that vacuum, health systems increasingly expand nonphysician roles. While nonphysicians are valuable team members, substitution is not restoration. Expertise cannot be redistributed by degree inflation. A sustainable workforce strategy must begin with retention—making it possible for physicians to remain in medicine without sacrificing health, family, or conscience (Figure 3).
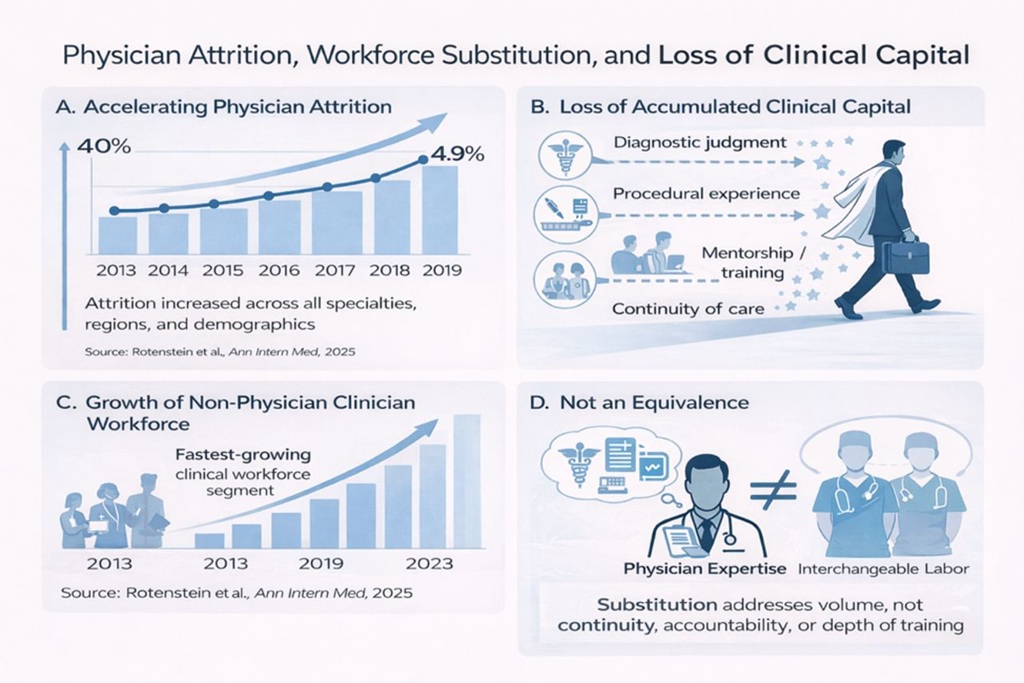
Figure 3
Rising physician attrition and workforce substitution. (A) Increasing attrition from clinical practice is associated with (B) loss of accumulated clinical capital and (C) concurrent expansion of the nonphysician clinician workforce. (D) While substitution may increase capacity, it does not replace the continuity, accountability, and depth of expertise lost through physician attrition.
The Call to Remember
Reimbursement is not merely a paycheck; it is a tangible measure of what society believes medical judgment is worth. When that value falls by a third, something larger than money is being lost. Incrementalism has failed. Silence has been the most expensive code of all.
Reform, Recognition, and Renewal
The current policy moment presents opportunity. Congressional scrutiny of CPT governance, debate over ACA subsidy extensions, and renewed focus on physician payment reform reflect growing recognition that the infrastructure of reimbursement itself must be examined.12,13
A reimagined payment framework—one that values judgment, supports independent practice where feasible, and aligns reimbursement with real costs and work—would benefit not only spine surgeons, but patients and the health care system as a whole. The challenges outlined here are not immutable. They are policy choices, and because they are choices, they can be changed.
Footnotes
- Funding The authors received no financial support for the research, authorship, and/or publication of this article.
- Declaration of Conflicting Interests The authors report no conflicts of interest in this work.
- Disclaimer The opinions shared in this essay are those of the authors and do not necessarily reflect the opinions of ISASS or this journal.
- Editor’s Note Morgan P. Lorio is a Past President of ISASS and Chair Emeritus of the ISASS Coding & Reimbursement Task Force. Kai-Uwe Lewandrowski is a Chief Deputy Editor of IJSS.
- This manuscript is generously published free of charge by ISASS, the International Society for the Advancement of Spine Surgery. Copyright © 2026 ISASS. To see more or order reprints or permissions, see http://ijssurgery.com.
References
- 1.↵ Haglin JM , Zabat MA , Richter KR , et al . Over 20 years of declining medicare reimbursement for spine surgeons: a temporal and geographic analysis from 2000 to 2021. J Neurosurg Spine. 2022;37(3):452–459. 10.3171/2022.2.SPINE211368 Google ScholarCrossRef
- 2.↵ Behm C . A path to ‘fair valuation’ in spine. Becker’s Hospital Review. December 5, 2025. https://www.beckershospitalreview.com/orthopedics/a-path-to-fair-valuation-in-spine.Google Scholar
- 3.↵ Dyrda L . Physicians in private practice drops to 46.7%. Becker’s Hospital Review. July 13, 2023. https://www.beckershospitalreview.com/hospital-transactions-and-valuation/physicians-in-private-practice-drop-to-46-7.Google Scholar
- 4.↵ Cassidy B . Letter to Bobby Mukkamala, M.D., President of the American Medical Association . US Senate Committee on Health, Education, Labor, and Pensions. October 6, 2025. https://www.help.senate.gov/imo/media/doc/cassidy_letter_to_ama_on_cpt_monopoly.pdf.Google Scholar
- 5.↵ Lorio MP . Navigating the future of spine surgery: a surgeon’s reflection on coding, reimbursement, and emerging technologies. Int J Spine Surg. 2024;18(2):120–121. 10.14444/8597 Google ScholarCrossRefFull TextPubMed
- 6.↵ US Senate Committee on Health, Education, Labor and Pensions . Chair Cassidy Rebukes AMA for Abusing CPT System, Raising Health Care Costs on American Families. October 8, 2025. https://www.help.senate.gov/rep/newsroom/press/chair-cassidy-rebukes-ama-for-abusing-cpt-system-raising-health-care-costs-on-american-families. 24 December 2025.Google Scholar
- 7.↵ American Medical Association . AMA 2024 Annual Report: Why We Fight! . https://www.ama-assn.org/system/files/2024-ama-annual-report.pdf. 23 December 2025.Google Scholar
- 8.↵ American College of Surgeons . Surgeon Risk of Mortality Is Highest Among All Physician Types . August 5, 2025. https://www.facs.org/for-medical-professionals/news-publications/news-and-articles/acs-brief/august-5-2025-issue/surgeon-risk-of-mortality-is-highest-among-all-physician-types.Google Scholar
- 9.↵ Patel VR , Stearns SA , Liu M , Tsai TC , Jena AB . Mortality among surgeons in the United States. JAMA Surg. 2025;160(9):1032–1034. 10.1001/jamasurg.2025.2482 Google ScholarCrossRef
- 10.↵ Henderson JV , Storeygard A , Weil DN . Measuring economic growth from outer space. Am Econ Rev. 2012;102(2):994–1028. 10.1257/aer.102.2.994 Google ScholarCrossRefPubMed
- 11.↵ Rotenstein LS , He Z , Dziura J , et al . Trends in and predictors of physician attrition from clinical practice across specialties : a nationwide, longitudinal analysis. Ann Intern Med. 2025;178(12):1698–1708. 10.7326/ANNALS-25-00564 Google ScholarCrossRef
- 12.↵ Chatterjee N . Congress is ending the year without a health care deal. What comes next? Time. December 21, 2025. https://time.com/7342062/health-care-costs-aca-subsidies-congress-2026/.Google Scholar
- 13.↵ U.S. Department of Health and Human Services . HHS Proposes Physician Payment Rule to Drive Whole-Person Care and Improve Health Quality for All Individuals with Medicare. 2024. https://www.cms.gov/newsroom/press-releases/hhs-proposes-physician-payment-rule-drive-whole-person-care-and-improve-health-quality-all?utm_source=chatgpt.com. 24 December 2025.Google Scholar