Elizabeth Hofheinz, M.P.H., M.Ed.

There is a lot to unpack in a recent massive study of patients with knee osteoarthritis (OA).
Using the National Ambulatory Medical Care Survey (NAMCS), a tool of the National Center for Health Statistics at the CDC, researchers set out to assess trends in opioid prescriptions for knee OA, determine which opioid-based medications were being prescribed for knee OA, and identify what patient- and provider-related factors influenced the prescribing of opioids in knee OA for outpatients.
The researchers looked at NAMCS data from 2007 to 2016 for all patients who presented to an outpatient clinic with any of the following primary issues: “knee symptoms”; “knee pain, ache, soreness, and discomfort;” “knee cramps, contractures, and spasms”; “weakness of the knee”; swelling of the knee”; “unspecified joint pain, ache, and soreness”; “unspecified joint cramps and contracture”; “arthritis”; “leg symptoms”; and “leg pain, ache soreness, and discomfort” AND were deemed to have an International Classification of Diseases (ICD), Ninth Revision or ICD, Tenth Revision diagnoses for knee arthritis
The study, “Addressing National Opioid Prescribing Practices for Knee Osteoarthritis: An Analysis of an Estimated 41,389,332 Patients With Knee Arthritis,” was published in the Journal of the American Academy of Orthopaedic Surgeons.
Co-author Ahmed K. Emara, M.D. of the Cleveland Clinic Foundation told OSN: “We were, and still are, seeing a hard-hitting opioid epidemic among patients with knee osteoarthritis. This challenge has persisted for over a decade despite the calls for improved prescription regulation and patterns of consumption.”
“We looked at patients who presented to ambulatory clinics nationwide, then identified those who received an opioid prescription for their knee pain. There were three notable findings.”
Change is slow
“A notable trend of decreased opioid prescription for knee osteoarthritis was only demonstrable as recent as 2013, while calls for action to provide better opioid regulation markedly predated this.”
Depressed patients: 225% more likely receive opioids for knee OA
“Several factors were associated with higher odds of being prescribed opioids for knee osteoarthritis pain including being evaluated by a non-orthopaedic provider, belonging to the lowest income quartile, having a worker’s comp insurance status or a concurrent diagnosis of depression.”
Tramadol on the rise
“While the most recent trends indicate a modest decrease in opioid-based medication prescription for knee osteoarthritis, a more granular analysis reveals a form of ‘drug substitution’ where traditional opioid medications are being replaced by tramadol. Providers should be cognizant that tramadol is not without its own set of complications and does pose an addictive potential.”
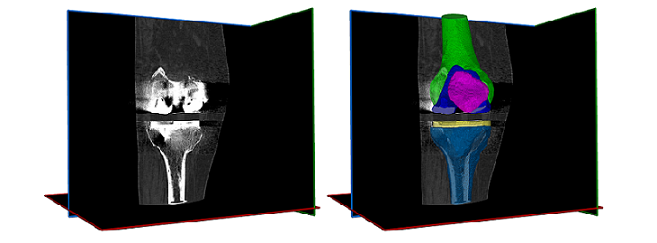
“Providers agree that opioid medications – while sometimes necessary – should not be a mainstream nonoperative management modality for arthritic knee pain. We need to revisit the risks vs. benefits of relatively earlier surgical intervention (mostly joint replacement) vs. prolonged use of opioid prescription, particularly among vulnerable or at-risk populations. This is particularly salient given that while opioid medications may provide pain control, they do not provide considerable functional improvement while posing several medical and surgical risks.”
Where to go from here
“One of the main challenges to evaluating a patient’s opioid use is difficulty determining who is an acute user, chronic user, or even abuser. Furthermore, details of consumption patterns could identify certain populations who are at elevated risk, despite having a similar cumulative dose and duration of use to other patients with more favorable/regulated use patterns. It is critical to view opioid – another prescription drug – use as a multifaceted, multidimensional challenge that requires a holistic evaluation that can also be evaluated scalarly for research and investigation.”
“One such metric is the Narx score; a newly adopted metric into patients’ charts that can help providers identify higher-risk patients to trigger a discussion rather than a unilateral decision. We have embarked upon further analyzing this metric and its association with postoperative complications to help our patients receive better care and safer surgery.”
Additional authors involved in the study were from: Wake Forest Baptist Health in Winston-Salem, North Carolina and Michigan State University in East Lansing.