Elizabeth Hofheinz, M.P.H., M.Ed.
Noting that incidental durotomy (ID)—a dural tear—can occur in up to 14% of lumbar spine surgeries, a team from the University of Virginia and the Johns Hopkins Hospital have published a review article looking at the varieties of treatment algorithms for this condition.
Their work, “Incidental Durotomy in Lumbar Spine Surgery; Risk Factors, Complications, and Perioperative Management,” appears in the March 15, 2021 edition of the Journal of the American Academy of Orthopaedic Surgeons.
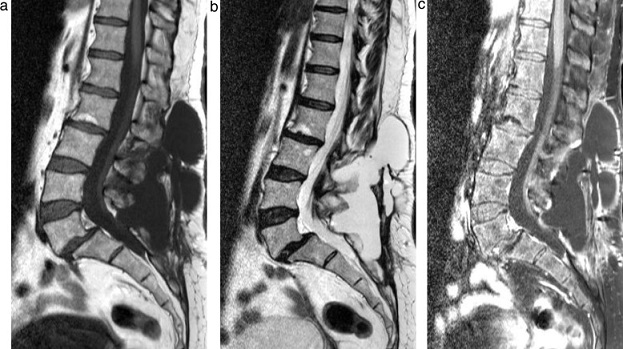
Pointing to the potential gravity of the situation, the authors wrote: “…The risk of this complication is markedly higher among elderly patients with advanced spinal pathology. In addition, revision cases and other more invasive procedures increase the risk of ID. When unrepaired, IDs can increase the risk of developing meningitis and can lead to the formation of cerebrospinal fluid fistulas and pseudomeningoceles…”
Co-author Hamid Hassanzadeh, M.D. is director of the Spine Fellowship and co-director of the Spine Center at the University of Virginia Medical Center Department of Orthopaedic Surgery. He told OSN, “Although incidental durotomy is a common complication during lumbar surgery, there exists a variety of treatment options among spine surgeons.”
The authors of this article, who indicate that the prevalence of incidental durotomy is climbing as the number and complexity of lumbar surgery increases, say that some aspects of current treatment algorithms include repair techniques, antibiotics and drains, and postoperative mobilization.
“Patients at the University of Virginia were treated with primary repair, subfacial drains and standard 24-hr postoperative antibiotics, and we saw few subsequent infections and revisions.”
“While primary suture repair is considered the gold standard,” said Dr. Hassanzadeh to OSN, “indirect repair alone has shown comparable patient outcomes. Moreover, subfacial drains and early ambulation have shown to promote wound healing and decrease rehabilitation time, respectively. However, there was little evidence supporting prolonged prophylactic antibiotics. Surgery with subfacial drains has shown to provide optimal outcome.”
The authors wrote, “Despite the high degree of inconsistency among drain protocols, subfascial drains have been shown to be a safe option in the postoperative management of ID, whereas there may be some utility with the addition of lumbar drains.”
The authors indicate that recent research has challenged the idea that prolonged bed rest (2 to 7 days) is best for these patients. Dr. Hassanzadeh said to OSN: “We also recommend early mobilization in asymptomatic patients, with additional bed rest for symptomatic patients.”
“Prospective studies are necessary to understand the impact of incidental durotomy on short- and long-term patient outcomes and cost.”