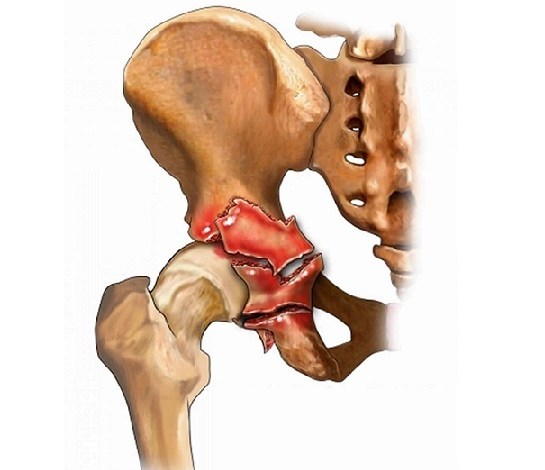
Topical Intrawound Antibiotic Powder Does NOT Reduce SSI Risk After Acetabular Fracture ORIF
Elizabeth Hofheinz, M.P.H., M.Ed.
Citing, in part, a rise in the marketing of antibiotic powders promising to reduce infection risk, a team of researchers from the University of Alabama at Birmingham (UAB) set out to clarify the efficacy of topical intrawound antibiotic powder.
Their work, “Intrawound Antibiotic Powder in Acetabular Fracture Open Reduction Internal Fixation Does Not Reduce Surgical Site Infections,” was published in the April 2021 edition of the Journal of Orthopaedic Trauma.
Elie Ghanem, M.D. is Assistant Professor of Orthopedics and Section Head of Total Joint Arthroplasty at the UAB. Dr. Ghanem told OSN: “Different solutions and powders are used routinely in orthopedic surgery nationwide with little evidence to support these practices. We perform an abundant amount of acetabular fracture surgeries at our institute with a high risk for infection. So naturally we wanted to address this lack of evidence in the literature utilizing our own institution’s experience.”
“There is so little data in the current literature at this point. Also, there has been an increase in solvents and powders being sold on the market being promoted as decreasing the risk of infections that we felt the need to bring this issue to light with hard evidence to add to the literature.”
For this retrospective cohort, performed at a Level I trauma center, the researchers included 789 acetabular fracture open reduction internal fixation (ORIF) cases from 2010 to 2019 (mean followup of 18 months). A total of 463 patients received topical antibiotic powder (294 vancomycin and 169 vancomycin/tobramycin), with 326 patients in the control group who received no such powder; the procedures were performed by 14 orthopedic trauma surgeons.
“The choice of surgical approach was dictated by the individual fracture classification and associated pelvic ring injuries, if present, at the discretion of the operating surgeon,” wrote the authors. “Anterior approaches included lateral window, modified Stoppa/anterior intrapelvic, and ilioinguinal, whereas posterior approaches included Kocher–Langenbeck and Gibson approaches.”
“…All patients received perioperative antibiotics within 1 hour of incision and were made non–weight-bearing or toe-touch weight-bearing with posterior hip precautions, when appropriate, postoperatively…”
Dr. Ghanem told OSN: “We found no difference in infection rates in these high-risk procedures using local antibiotic powder in the wound prior to closure.”
Looking forward, Dr. Ghanem commented to OTW, “We would conduct large multicenter studies with 20-40 centers over a long period of time in order to maximize the power of the study.”
“When introducing new measures to decrease infection including the use of antibiotics in the wound or solvents, we need to critically assess their effects in large studies and then conduct a meta-analysis to pool these studies in order to come to a conclusion on their efficacy. Unfortunately, this is not being done to the extent it should and more clinical trials and retrospective studies are required to shed light on this important topic.”





