Elizabeth Hofheinz, M.P.H., M.Ed.
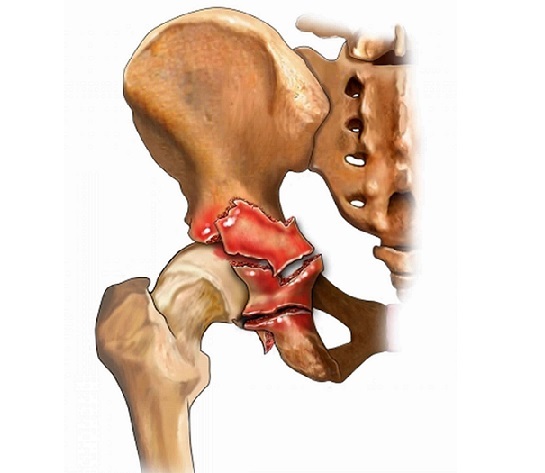
New work performed at eight academic Level 1 trauma centers has looked at whether patients with positive intraoperative cultures for infected nonunions are more likely to have persistent nonunion than those with negative cultures.
Their study, “The Fate of Patients After a Staged Nonunion Procedure for Known Infection,” appears in the April 2021 edition of the Journal of Orthopaedic Trauma.
One co-author was Paul Tornetta III, M.D., Chief and Chair, Professor and Residency Program Director in the Department of Orthopaedic Surgery at Boston University School of Medicine and the Director of Orthopaedic Trauma for the Boston Medical Center. Dr. Tornetta commented to OSN, “There was not a great deal of data on staged reconstructions for obviously infected nonunions. In particular, we, and others have found that in other not obviously infected nonunions a positive culture from the definitive surgery was a negative predictor of successful union with one operation. We wanted to explore this in a group of staged reconstructions.”
Using data from 134 patients treated with staged procedures for obviously infected nonunion of a long bone, the researchers reviewed initial fracture management, management of retained implants, number of debridements, grafting, bacteriology, antibiotic course, bone defect management, soft-tissue coverage, and definitive surgery performed.
The authors defined “staged management” as “treatment of an infected nonunion with at least 1 procedure aimed at eradicating the infection and a second procedure aimed at definitive fixation to achieve fracture union. Infection was diagnosed either preoperatively or intra-operatively in all cases by the treating surgeon, and an infected nonunion was defined as a failure to gain union 6 months after initial treatment for the index injury with persistent infection at the fracture site.”
“During definitive procedures, 120 patients had intraoperative cultures taken with 43% having positive cultures. For culture-positive patients, 41 patients achieved eventual union and 10 had persistent nonunion,” wrote the authors. “Of 69 culture-negative patients, 66 achieved eventual union and 3 had persistent nonunion. The number of patients with union versus persistent nonunion was statistically significant between culture- positive and culture-negative groups (P = 0.015).”
Clear need for a standard protocol
“Patients with positive cultures from the time of the definitive surgery have a lower rate of successful union than those with negative cultures, even if these are treated with antibiotics,” said Dr. Tornetta to OSN. “We now need more information about ways to determine the presence of bacteria at the nonunion site in real time in the OR. Otherwise, patients may require biopsy negativity prior to definitive reconstruction, which may, in and of itself, be a risk factor for failure.”