Biogennix, November 8, 2022 – OrthoSpineNews – Featured Article
Biologically active bone grafts are being increasingly favored by surgeons due to their advanced properties and their ability to positively influence healing. While different bone graft materials have different mechanisms of interacting with cells, all biologically active graft materials are similar in that they play an active role in the bone formation process and can positively influence cellular healing. This article explains the different mechanisms through which biologically active graft materials play an active role in healing.
Biologically Active Bone Grafts: Same Result, Different Mechanism of Action
Before we dive into the different mechanisms of action for biologically active bone grafts, it’s important to understand some basics.
The core property of all bone grafts is osteoconductivity. Osteoconductivity is the ability of a material to function as a scaffold that supports bone formation on its surface. In bone graft surgical applications, this is a vital requirement in the bone regeneration response. Without a scaffold, new bone has nowhere to form and the graft site will not heal. Due to the importance of osteoconductivity in bone graft function, this was the main feature of many first-generation bone graft products. However, grafts that are solely osteoconductive, with no advanced properties, are limited to playing a passive role in the bone formation process.
More advanced bone graft materials are osteoconductive, but also possess properties that can positively influence and accelerate the bone formation response, making them biologically active in the healing process. A description of some of the most common biologically active materials and their mechanism of action is described below.
Demineralized Bone Matrix – DBM (Allograft)
Products containing demineralized bone matrix (DBM) can show biological activity. Bone naturally contains a variety of protein-based growth factors that are capable of stimulating osteoblast proliferation and function and cause stem cell differentiation (osteoinductivity). However, in bone’s natural state these osteoinductive proteins are trapped in the mineralized collagen matrix. In DBM tissue processing, ground cortical bone (or cancellous blocks) is exposed to acid to remove the bone mineral while retaining the collagen and growth factor proteins. This process exposes the trapped growth factors and, once implanted, allows them to be released from DBM and interact with cells.
However, the osteoinductive ability of DBM is highly sensitive to processing, product formulation, and sterilization. Advanced DBM products that are designed to maintain DBM osteoinductivity can positively influence the cellular bone formation process through these growth factor proteins. As such the mechanism of action for bone grafts like advanced DBM allograft can be thought of as protein stimulation.
Bone Morphogenetic Protein-2 (Growth Factor)
The initial investigation of DBM identified a variety of proteins within bone tissue. In particular, one class of proteins, called “bone morphogenetic protein” (BMP), was discovered to play a significant role in the bone formation process. Multiple BMP proteins (BMP-1 through BMP-14) were subsequently identified and isolated based on their ability to stimulate the bone healing process. In particular, a recombinant version of bone morphogenetic protein-2 (rhBMP-2) has become a widely used bone grafting product. Similar to DBM, BMP-2 can stimulate osteoblast function and cause stem cell differentiation.
Bioactive Glass
Bioactive glass, or Bioglass, was one of the earliest synthetic (non-human tissue-based) bone graft products to be considered biologically active. Bioglass is a resorbable glass with unique properties that improve the bone formation response. Once Bioglass is implanted, it undergoes an aqueous dissolution process that releases ions to the surrounding area. These ions can stimulate cellular healing (increase in osteoblast function and stem cell differentiation) and also allow the formation of a mineral surface on the glass (bioactivity). The mechanism of action for bone grafts like bioactive glass can be thought of as ion stimulation.
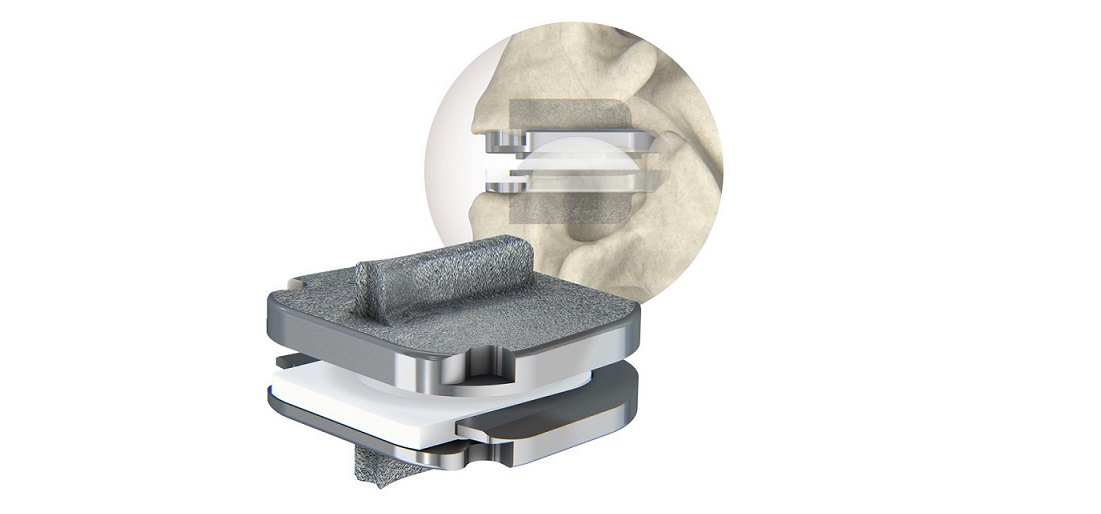
Next-Generation Synthetic Bone Grafts
Advancements in biomaterials have resulted in the development of next-generation synthetic bone graft products, different from Bioglass, that play an active role in the bone formation process. Next-generation synthetic bone grafts do this through a mechanism that involves their surface morphology and surface composition.
Surface Morphology-Various studies on surface morphology have shown that synthetic materials with nano-sized surface features can increase osteoblast function and result in stem cell differentiation (Zhang, 2017; Duan, 2018). This occurs early in the bone healing process as cells initially attach to the nano-structured surface. Other studies on bone graft composition have shown that the bone formation response can be accelerated based on material composition.
Surface Composition-Typical synthetic bone graft materials based on calcium phosphate (e.g., hydroxyapatite – HA and tricalcium phosphate – TCP) undergo a cellular preparation phase prior to the start of the bone formation process. One material, hydroxycarbanoapatite (HCA), has been shown to have a significantly shortened preparation phase due to its similarity to bone mineral. Testing showed that HCA materials resulted in significantly faster bone formation than HA or TCP (Hyashi, 2019).
Advanced synthetic bone graft materials represent an improvement over passive bone graft materials that are based on first-generation technology. Advanced synthetics have the potential to produce better patient outcomes than earlier synthetic products, as they offer regeneration-influencing surface morphology and composition. Surface composition and surface morphology can be considered the third mechanism of action for bone grafts that are biologically active.
Additionally, because of their advanced features, next-generation synthetic materials offer many of the same benefits of allograft and growth factor products, while mitigating the risks associated with human tissue products. Surgeons have been increasingly drawn to these benefits, as evidenced by the growing market shift towards advanced synthetic bone graft products.
Choosing the Right Material
As seen from the various mechanisms of biological activity in bone grafts, the end result is an improvement to the bone formation response. Human tissue-based products, like DBMs and growth factor products, influence cells through protein stimulation. Bioglass products influence cells through ion release. Newer, advanced synthetic bone graft products do the same through their nano-structured surfaces and bone-like compositions. By understanding the different mechanisms of action for bone graft materials that are biologically active, surgeons can consider the risks and benefits of each type of product and decide which is best for their patient.
Biogennix is committed to delivering next-generation technologies that improve clinical outcomes. Our full line-up of TrelCor® bone graft products features advanced material properties that positively influence cell attachment and differentiation and encourage healing to begin sooner than with other synthetic materials. To learn more about Biogennix next-generation bone graft solutions, contact our team today.
As a recognized leader in advanced bone graft technologies, Biogennix is committed to bringing high-quality educational content to our field. This blog will cover technical topics ranging from basic bone graft science to advanced osteobiologic principles. We’ll also discuss market trends and industry challenges. We thank you for reading and invite you to learn more about us here.
Contact: info@biogennix.com